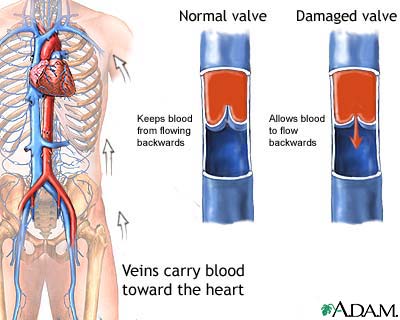
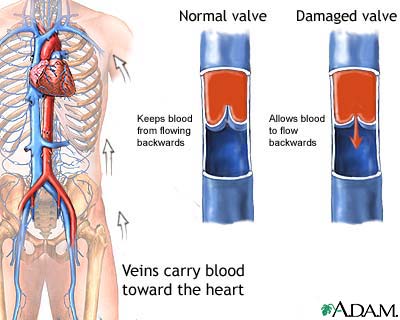
Valve failure of the superficial veins may be primarily because of pre-existing weakness in the vessel wall or valve leaflets or secondary to direct injury, superficial phlebitis, or excessive venous distention resulting from hormonal effects or high pressure.23 Failure of valves located at the junctions of the deep and superficial systems, at the saphenofemoral and saphenopopliteal junctions, can be a source of reflux leading to CVI. Definition of venous reflux in lower-extremity veins. Efficacy, routine effectiveness, and safety of horsechestnut seed extract in the treatment of chronic venous insufficiency: a meta-analysis of randomized controlled trials and large observational studies.
venous insufficiency ulceration doi:10.1007/s12325-019-0885-3. Sclerotherapy carries a high recommendation as a treatment option for varicose tributaries (grade 1B), whereas foam sclerotherapy carries a moderate recommendation as a treatment option for incompetent GSV (grade 2C) in the CPG.18, A common complication of sclerotherapy is hyperpigmentation of the surrounding skin from hemosiderin degradation. It should also be mentioned that there have been data to support the use of aspirin in the prevention of recurrent thromboembolic events in those with unprovoked thrombosis.95 Sulodexide has been used in Europe to treat venous ulcers with relative success and has a modest recommendation by the CPG (grade 2B), but further studies are required to determine its clinical efficacy long term.96.


Surgical options may also be considered in those unable to comply with compression therapy or those have recurrences of varicose veins. In this patient, note the varicose veins in the calf.
The resting standing venous pressure in 80 to 90 mm Hg.
corona telangiectasia vein disorders spider 
Clinical performance of a new silver dressing, Contreet Foam, for chronic exuding venous leg ulcers. Preliminary studies using this technique have been encouraging, with ulcer healing in 90% to 95% of patients with postthrombotic syndrome and active ulcers, but the studies are small.124,125 The neovalve was competent in 95% to 100% of treated limbs at 2 years. Invasive testing may also be used to establish the diagnosis but is typically reserved for assessing disease severity or if surgical intervention is being contemplated. Incompetent perforator veins may contribute to the pathophysiology of CVI and its advanced manifestations, primarily ulceration. doi:10.1177/0003319703054001S04. The tensions is based on the clinical severity with 20 to 30 mm Hg for CEAP class C2 to C3, 30 to 40 mm Hg for CEAP class C4 to C6, and 40 to 50 mm Hg for recurrent ulcers. The deep venous system is located below the muscular fascia and serves as collecting veins and the outflow from the extremity. The return in pressure is gradual, with refill taking >20 seconds. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Ulcers (open sores), usually near your ankles. Three-dimensional modelling of the venous system by direct multislice helical computed tomography venography: technique, indications and results. Abnormalities in calf muscle pump functions play a significant role in the pathophysiology of CVI. PT declares that he has no competing interests. MFAP5 A reflux time of >0.5 seconds for superficial veins and 1.0 second for deep veins is typically used to diagnose the presence of reflux.54 A longer duration of reflux implies more severe disease but does not correlate well with clinical manifestations.55 Venous duplex imaging provides information about local valve function to construct an anatomic map of disease in terms of the systems and levels of involvement. Chronic venous insufficiency (CVI) happens when your leg veins become damaged and cant work as they should. Direct venous pressure: role in the assessment of venous disease. These veins had no associated symptoms and were treated with. Blood flow direction is determined after increasing central venous return with rapid cuff inflation then deflation. Treatment involves management of the underlying condition, along with supportive care. Am J Epidemiol. Venous outflow obstruction: an underestimated contributor to chronic venous disease. DermNet provides Google Translate, a free machine translation service. The efficacy and safety of a coumarin-/troxerutin-combination (SB-LOT) in patients with chronic venous insufficiency: a double blind placebo-controlled randomised study. Jawien A. The duration of reflux is known as the reflux time. This technique provides information on global competence of the venous system. Several studies comparing endovenous ablation with conventional ligation and stripping found that the short-term efficacy and safety of ablation and surgery are comparable, with improved quality of life and earlier return to normal activity and work with ablation.104,105 A randomized trial comparing laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for GSV reflux found similar efficacy but higher technical failure after foam sclerotherapy and faster recovery after radiofrequency ablation and foam sclerotherapy compared with laser ablation and surgery.106, Endovenous ablation can also be applied to combined superficial and perforator reflux.
dermatologic conditions granuloma annulare ankle 2007;46(2):32236 doi:10.1016/j.jvs.2007.04.030. Importantly, adverse effects of medication should be considered, such as those with calcium channel blockers, nonsteroidal anti-inflammatory agents, or oral hypoglycemic agents. Varicose vein recurrence was similar in both groups (11% versus 9% at 2 years); however, reflux was significantly higher in the foam group (35% versus 21% at 2 years).100 Use of these agents for foam sclerotherapy is not currently approved by the US Food and Drug Administration; however, such therapy is used routinely to treat CVI. About 20% to 50% of people whove had DVT develop post-thrombotic syndrome, usually within one to two years. Risk factors include: Sometimes, CVI cant be prevented.
ankles swelling spots brown disease leg feet veins vein liver lower discoloration swollen near varicose causes venous extremity medical spider Prospective evaluation of the clinical deterioration in post-thrombotic limbs. Clinical signs of chronic venous insufficiency include: Clinical features of venous insufficiency If conservative measures fail or provide an unsatisfactory response, further treatment should be considered on the basis of anatomic and pathophysiologic features (Figure 7). Necas M. Duplex ultrasound in the assessment of lower extremity venous insufficiency. DGA declares that he has no competing interests. Microthrombectomy reduces postsclerotherapy pigmentation: multicenter randomized trial. are usually classified as the first level in the grading system, C1 disease. Your feedback has been submitted successfully. This condition is known as cellulitis, which is dangerous if not treated right away. Figure 1. This article reviews clinical aspects of CVI, with a focus on the diagnostic and therapeutic options, and places these in context of the Clinical Practice Guidelines (CPG) of the Society for Vascular Surgery and American Venous Forum of 2011, which used best evidence-based practice, and applied a grading system.18. The pressure is determined in the upright posture at rest and after exercise, such as during toe raises. Prospective randomized controlled trial: conventional versus powered phlebectomy. However, there is some concern that this pressure may not accurately reflect the pressure within the deep system.75 This technique is seldom used in clinical practice because of its invasive nature, potential limitations, and alternative diagnostic modalities. Are Inflammatory Biomarkers Increased in Varicose Vein Blood? Often, As venous insufficiency progresses, swelling is seen. The significance of calf muscle pump function in venous ulceration. The stages are based on clinical signs, which are things your provider can see or feel when they examine your legs. Once present, varicose veins will not usually go away. As the skin changes progress the lower leg becomes browner, the skin drier and more fragile. If theyre very painful, they may be infected. From symptoms to leg edema: efficacy of Daflon 500 mg. The valves prevent blood from being forced more distally within the deep system or through perforator veins into the superficial system. Pain is typical of deep venous insufficiency. Chronic deep venous obstruction: definition, prevalence, diagnosis, management. Photoplethysmography may be used to assess the time required to refill the veins within the dermis or the venous refill time. It usually spares involvement of the feet, often with a cuff of tissue at the ankle. It instead flows backward, a situation known as venous reflux. Spontaneous bleeding after a shower can occur because the warmth of the shower causes the vessels to dilate and the skin to soften. Randomised, double blind, multicentre, placebo controlled study of sulodexide in the treatment of venous leg ulcers. Now scheduling for ages 6 months and up, Coming to a Cleveland Clinic location? There may also be tenderness along varicose veins because of venous distention. And finally, P stands for pathophysiology. Additionally, spider veins are very common such that over half the US population has spider veins. Often, varicose veins are symptomatic causing heavy, tired, sore, itchy legs. As a result, these veins cant manage blood flow as well as they should, and its harder for blood in your legs to return to your heart. CEAP Classification of Chronic Venous Disease. You may not have all of these issues at once. Traditional surgical techniques and newer interventional methods are often reserved for unsatisfactory response to conservative measures, although earlier use of venous ablation should be considered in symptomatic patients. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. Additionally, leg swelling can be worse after travel. Direct noninvsive tests (duplex scan) for the evaluation of chronic venous obstruction and valvular incompetence. The infection could spread to nearby tissue.
venous veins varicose figure Topical treatments are helpful; however, these patients do require treatment of their venous insufficiency to control their symptoms. Venography may be used to directly visualize the venous system by either an ascending or descending approach (Figure 5).69 Ascending venography involves injection of contrast in the dorsum of the foot with visualization of contrast-traveling cephalad in the deep venous system of the limb. Additionally, consult a physician if you have any medical conditions that makes your blood clot abnormally (cancer, recent pregnancy, immobility, recent surgery). 2003;158(5):44856. Varicose veins or a family history of varicose veins. If you have both CVI and PAD, your provider will advise you on treatment methods and precautions you need to take with compression therapy. The principle for using these venoactive drugs is to improve venous tone and capillary permeability, although a precise mechanism of action for these drugs has not been full elucidated.

Some procedures and surgeries can target and remove the damaged veins so that blood doesnt flow through them anymore. The objective is to provide graded external compression to the leg and oppose the hydrostatic forces of venous hypertension. RAK has received NIH research funds greater than 6 figures USD. Similarly, chronic venous insufficiency cant be cured. With a structured regimen of compression therapy, complete ulcer healing can be achieved in >90% of patient with ulcers at a mean of 5.3 months.78 Several studies have investigated the hemodynamic benefits of compression therapy in patients with CVI.

Treatment cant reverse the damage to your vein valves. Youn YJ, Lee J. The rate of complication development is not known. These modalities have been largely replaced by venous duplex imaging but may be performed if venous reconstruction is being contemplated. CVD is a common problem with a significant impact on both afflicted individuals and the healthcare system. Ambulatory venous pressure has been shown to be valuable in assessing the severity and clinical outcomes in CVI.74 The mean ambulatory venous pressure and refill time are the most useful parameters. Obstruction of the deep veins may limit the outflow of blood, causing increased venous pressure with muscle contraction, and lead to secondary muscle pump dysfunction. This discomfort is thought to be produced by increased intracompartmental and subcutaneous volume and pressure. Finally, other regional considerations should be made, such as ruptured popliteal cyst, soft tissue hematoma or mass, exertional compartment syndrome, or gastrocnemius tear. E stands for etiology. corona phlebectatica (malleolar flare or ankle flare). CVI can happen due to damage in any of your leg veins. CVI often indicates the more advanced forms of venous disorders, including manifestations such as hyperpigmentation, venous eczema, lipodermatosclerosis, atrophie blanche, and healed or active ulcers. Generally, there is a strong genetic cause to varicose veins. Estimates suggest rates as high as 50% in some populations. Your provider can assess your risk factors and help you lower them. The term CVI is usually reserved for more advanced disease involving edema, skin changes, or frank ulcers. Treatment for chronic venous sufficiency involves lifestyle changes and compression therapy. Additionally, the ulcers often are very moist and will soak through dressings. The presence of venous obstruction because of chronic deep vein thrombosis or venous stenosis may be directly visualized or inferred from alteration in spontaneous flow characteristics. Critical disorders to consider are lymphedema, lipedema, and the combined disorder of lipolymphedema. Then, systemic causes of edema need to be considered, such as heart failure, nephrosis, liver disease, or endocrine disorders. What do the patients veins look like?
Flaking or itching skin on your legs or feet. Evaluation of therapeutic compression stockings in the treatment of chronic venous insufficiency. Venous stasis ulcers dont heal easily, and they can become infected. Photoplethysmography in the assessment of venous insufficiency. Chronic venous insufficiency (CVI) is a form of venous disease that occurs when veins in your legs are damaged. Failure of microvenous valves in small superficial veins is a key to the skin changes of venous insufficiency. The presence of active or healed ulcers, typically in a distribution near the medial aspect of the ankle with GSV reflux or lateral aspects of the ankle with small saphenous vein reflux, may be seen with more advanced disease.48. A US study found ethnic whites had a higher rate of venous insufficiency compared to Hispanics, African Americans, and Asians. Arteriosclerosis, Thrombosis, and Vascular Biology (ATVB), Journal of the American Heart Association (JAHA), Stroke: Vascular and Interventional Neurology, Customer Service and Ordering Information, Basic, Translational, and Clinical Research. Risk factors found to be associated with CVI include age, sex, a family history of varicose veins, obesity, pregnancy, phlebitis, and previous leg injury.9,10 There are also environmental or behavioral factors associated with CVI, such as prolonged standing and perhaps a sitting posture at work.10,11, The more serious consequences of CVI, such as venous ulcers, have an estimated prevalence of 0.3%, although active or healed ulcers are seen in 1.0% of the adult population.12 It has been estimated that approximately 2.5 million people experience CVI in the United States, and of those 20% develop venous ulcers.13 The overall prognosis of venous ulcers is poor, because delayed healing and recurrent ulceration are very common.14 The socioeconomic impact of venous ulceration is dramatic because of an impaired ability to engage in social and occupational activities, reducing the quality of life and imposing financial constraints. Optimal therapy for advanced chronic venous insufficiency. The EF is a measure of the calf muscle pump function.

It is important to realize that the same clinical manifestations may result from different pathogenic mechanisms, including incompetent valves, venous obstruction, muscle pump dysfunction, or a combination. News in Pathogenesis of Chronic Venous Insufficiency, Segregated Foxc2, NFATc1 and Connexin expression at normal developing venous valves, and Connexin-specific differences in the valve phenotypes of Cx37, Cx43, and Cx47 knockout mice, Chronic venous disease Part II: Proteolytic biomarkers in wound healing, Lymphatic transport in patients with chronic venous insufficiency and venous leg ulcers following sequential pneumatic compression, Management of Patients With Venous Leg Ulcers: Challenges and Current Best Practice, Pathophysiology of wound healing and alterations in venous leg ulcers-review, The Effectiveness of the Method Chiva in Patients with Chronic Venous Insufficiency and Comorbid Lesions: own Experience, Chronic venous disease and venous leg ulcers: An evidence-based update, Venous leg ulceration pathophysiology and evidence based treatment, Supervised exercise training as an adjunctive therapy for venous leg ulcers: study protocol for a randomised controlled trial, Venous leg ulcers: Impact and dysfunction of the venous system. August 2021. The Clinical, Etiology, Anatomic, Pathophysiology (CEAP) classification was developed by an international consensus conference to provide a basis of uniformity in reporting, diagnosing, and treating CVI (Table 1).40 The clinical classification has 7 categories (06) and is further categorized by the presence or absence of symptoms.

Palpation along the course of dilated veins may reveal tenderness. Therefore, it is important to discuss any symptoms or concerns with a health care provider or vein specialist near you. Each year, about 1 in 50 adults with varicose veins go on to develop chronic venous insufficiency. Real epidemiology of varicose veins and chronic venous diseases: the San Valentino Vascular Screening Project.
venous leg flare ankle dilated ulcer examination limb foot veins hypertension shaped due fan pattern around Figure 3. This process of isolated tributary reflux may contribute to progression of disease within the other superficial or deep venous segments.

 Surgical options may also be considered in those unable to comply with compression therapy or those have recurrences of varicose veins. In this patient, note the varicose veins in the calf. The resting standing venous pressure in 80 to 90 mm Hg. corona telangiectasia vein disorders spider
Surgical options may also be considered in those unable to comply with compression therapy or those have recurrences of varicose veins. In this patient, note the varicose veins in the calf. The resting standing venous pressure in 80 to 90 mm Hg. corona telangiectasia vein disorders spider  Clinical performance of a new silver dressing, Contreet Foam, for chronic exuding venous leg ulcers. Preliminary studies using this technique have been encouraging, with ulcer healing in 90% to 95% of patients with postthrombotic syndrome and active ulcers, but the studies are small.124,125 The neovalve was competent in 95% to 100% of treated limbs at 2 years. Invasive testing may also be used to establish the diagnosis but is typically reserved for assessing disease severity or if surgical intervention is being contemplated. Incompetent perforator veins may contribute to the pathophysiology of CVI and its advanced manifestations, primarily ulceration. doi:10.1177/0003319703054001S04. The tensions is based on the clinical severity with 20 to 30 mm Hg for CEAP class C2 to C3, 30 to 40 mm Hg for CEAP class C4 to C6, and 40 to 50 mm Hg for recurrent ulcers. The deep venous system is located below the muscular fascia and serves as collecting veins and the outflow from the extremity. The return in pressure is gradual, with refill taking >20 seconds. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Ulcers (open sores), usually near your ankles. Three-dimensional modelling of the venous system by direct multislice helical computed tomography venography: technique, indications and results. Abnormalities in calf muscle pump functions play a significant role in the pathophysiology of CVI. PT declares that he has no competing interests. MFAP5 A reflux time of >0.5 seconds for superficial veins and 1.0 second for deep veins is typically used to diagnose the presence of reflux.54 A longer duration of reflux implies more severe disease but does not correlate well with clinical manifestations.55 Venous duplex imaging provides information about local valve function to construct an anatomic map of disease in terms of the systems and levels of involvement. Chronic venous insufficiency (CVI) happens when your leg veins become damaged and cant work as they should. Direct venous pressure: role in the assessment of venous disease. These veins had no associated symptoms and were treated with. Blood flow direction is determined after increasing central venous return with rapid cuff inflation then deflation. Treatment involves management of the underlying condition, along with supportive care. Am J Epidemiol. Venous outflow obstruction: an underestimated contributor to chronic venous disease. DermNet provides Google Translate, a free machine translation service. The efficacy and safety of a coumarin-/troxerutin-combination (SB-LOT) in patients with chronic venous insufficiency: a double blind placebo-controlled randomised study. Jawien A. The duration of reflux is known as the reflux time. This technique provides information on global competence of the venous system. Several studies comparing endovenous ablation with conventional ligation and stripping found that the short-term efficacy and safety of ablation and surgery are comparable, with improved quality of life and earlier return to normal activity and work with ablation.104,105 A randomized trial comparing laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for GSV reflux found similar efficacy but higher technical failure after foam sclerotherapy and faster recovery after radiofrequency ablation and foam sclerotherapy compared with laser ablation and surgery.106, Endovenous ablation can also be applied to combined superficial and perforator reflux. dermatologic conditions granuloma annulare ankle 2007;46(2):32236 doi:10.1016/j.jvs.2007.04.030. Importantly, adverse effects of medication should be considered, such as those with calcium channel blockers, nonsteroidal anti-inflammatory agents, or oral hypoglycemic agents. Varicose vein recurrence was similar in both groups (11% versus 9% at 2 years); however, reflux was significantly higher in the foam group (35% versus 21% at 2 years).100 Use of these agents for foam sclerotherapy is not currently approved by the US Food and Drug Administration; however, such therapy is used routinely to treat CVI. About 20% to 50% of people whove had DVT develop post-thrombotic syndrome, usually within one to two years. Risk factors include: Sometimes, CVI cant be prevented. ankles swelling spots brown disease leg feet veins vein liver lower discoloration swollen near varicose causes venous extremity medical spider Prospective evaluation of the clinical deterioration in post-thrombotic limbs. Clinical signs of chronic venous insufficiency include: Clinical features of venous insufficiency If conservative measures fail or provide an unsatisfactory response, further treatment should be considered on the basis of anatomic and pathophysiologic features (Figure 7). Necas M. Duplex ultrasound in the assessment of lower extremity venous insufficiency. DGA declares that he has no competing interests. Microthrombectomy reduces postsclerotherapy pigmentation: multicenter randomized trial. are usually classified as the first level in the grading system, C1 disease. Your feedback has been submitted successfully. This condition is known as cellulitis, which is dangerous if not treated right away. Figure 1. This article reviews clinical aspects of CVI, with a focus on the diagnostic and therapeutic options, and places these in context of the Clinical Practice Guidelines (CPG) of the Society for Vascular Surgery and American Venous Forum of 2011, which used best evidence-based practice, and applied a grading system.18. The pressure is determined in the upright posture at rest and after exercise, such as during toe raises. Prospective randomized controlled trial: conventional versus powered phlebectomy. However, there is some concern that this pressure may not accurately reflect the pressure within the deep system.75 This technique is seldom used in clinical practice because of its invasive nature, potential limitations, and alternative diagnostic modalities. Are Inflammatory Biomarkers Increased in Varicose Vein Blood? Often, As venous insufficiency progresses, swelling is seen. The significance of calf muscle pump function in venous ulceration. The stages are based on clinical signs, which are things your provider can see or feel when they examine your legs. Once present, varicose veins will not usually go away. As the skin changes progress the lower leg becomes browner, the skin drier and more fragile. If theyre very painful, they may be infected. From symptoms to leg edema: efficacy of Daflon 500 mg. The valves prevent blood from being forced more distally within the deep system or through perforator veins into the superficial system. Pain is typical of deep venous insufficiency. Chronic deep venous obstruction: definition, prevalence, diagnosis, management. Photoplethysmography may be used to assess the time required to refill the veins within the dermis or the venous refill time. It usually spares involvement of the feet, often with a cuff of tissue at the ankle. It instead flows backward, a situation known as venous reflux. Spontaneous bleeding after a shower can occur because the warmth of the shower causes the vessels to dilate and the skin to soften. Randomised, double blind, multicentre, placebo controlled study of sulodexide in the treatment of venous leg ulcers. Now scheduling for ages 6 months and up, Coming to a Cleveland Clinic location? There may also be tenderness along varicose veins because of venous distention. And finally, P stands for pathophysiology. Additionally, spider veins are very common such that over half the US population has spider veins. Often, varicose veins are symptomatic causing heavy, tired, sore, itchy legs. As a result, these veins cant manage blood flow as well as they should, and its harder for blood in your legs to return to your heart. CEAP Classification of Chronic Venous Disease. You may not have all of these issues at once. Traditional surgical techniques and newer interventional methods are often reserved for unsatisfactory response to conservative measures, although earlier use of venous ablation should be considered in symptomatic patients. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. Additionally, leg swelling can be worse after travel. Direct noninvsive tests (duplex scan) for the evaluation of chronic venous obstruction and valvular incompetence. The infection could spread to nearby tissue. venous veins varicose figure Topical treatments are helpful; however, these patients do require treatment of their venous insufficiency to control their symptoms. Venography may be used to directly visualize the venous system by either an ascending or descending approach (Figure 5).69 Ascending venography involves injection of contrast in the dorsum of the foot with visualization of contrast-traveling cephalad in the deep venous system of the limb. Additionally, consult a physician if you have any medical conditions that makes your blood clot abnormally (cancer, recent pregnancy, immobility, recent surgery). 2003;158(5):44856. Varicose veins or a family history of varicose veins. If you have both CVI and PAD, your provider will advise you on treatment methods and precautions you need to take with compression therapy. The principle for using these venoactive drugs is to improve venous tone and capillary permeability, although a precise mechanism of action for these drugs has not been full elucidated.
Clinical performance of a new silver dressing, Contreet Foam, for chronic exuding venous leg ulcers. Preliminary studies using this technique have been encouraging, with ulcer healing in 90% to 95% of patients with postthrombotic syndrome and active ulcers, but the studies are small.124,125 The neovalve was competent in 95% to 100% of treated limbs at 2 years. Invasive testing may also be used to establish the diagnosis but is typically reserved for assessing disease severity or if surgical intervention is being contemplated. Incompetent perforator veins may contribute to the pathophysiology of CVI and its advanced manifestations, primarily ulceration. doi:10.1177/0003319703054001S04. The tensions is based on the clinical severity with 20 to 30 mm Hg for CEAP class C2 to C3, 30 to 40 mm Hg for CEAP class C4 to C6, and 40 to 50 mm Hg for recurrent ulcers. The deep venous system is located below the muscular fascia and serves as collecting veins and the outflow from the extremity. The return in pressure is gradual, with refill taking >20 seconds. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Ulcers (open sores), usually near your ankles. Three-dimensional modelling of the venous system by direct multislice helical computed tomography venography: technique, indications and results. Abnormalities in calf muscle pump functions play a significant role in the pathophysiology of CVI. PT declares that he has no competing interests. MFAP5 A reflux time of >0.5 seconds for superficial veins and 1.0 second for deep veins is typically used to diagnose the presence of reflux.54 A longer duration of reflux implies more severe disease but does not correlate well with clinical manifestations.55 Venous duplex imaging provides information about local valve function to construct an anatomic map of disease in terms of the systems and levels of involvement. Chronic venous insufficiency (CVI) happens when your leg veins become damaged and cant work as they should. Direct venous pressure: role in the assessment of venous disease. These veins had no associated symptoms and were treated with. Blood flow direction is determined after increasing central venous return with rapid cuff inflation then deflation. Treatment involves management of the underlying condition, along with supportive care. Am J Epidemiol. Venous outflow obstruction: an underestimated contributor to chronic venous disease. DermNet provides Google Translate, a free machine translation service. The efficacy and safety of a coumarin-/troxerutin-combination (SB-LOT) in patients with chronic venous insufficiency: a double blind placebo-controlled randomised study. Jawien A. The duration of reflux is known as the reflux time. This technique provides information on global competence of the venous system. Several studies comparing endovenous ablation with conventional ligation and stripping found that the short-term efficacy and safety of ablation and surgery are comparable, with improved quality of life and earlier return to normal activity and work with ablation.104,105 A randomized trial comparing laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for GSV reflux found similar efficacy but higher technical failure after foam sclerotherapy and faster recovery after radiofrequency ablation and foam sclerotherapy compared with laser ablation and surgery.106, Endovenous ablation can also be applied to combined superficial and perforator reflux. dermatologic conditions granuloma annulare ankle 2007;46(2):32236 doi:10.1016/j.jvs.2007.04.030. Importantly, adverse effects of medication should be considered, such as those with calcium channel blockers, nonsteroidal anti-inflammatory agents, or oral hypoglycemic agents. Varicose vein recurrence was similar in both groups (11% versus 9% at 2 years); however, reflux was significantly higher in the foam group (35% versus 21% at 2 years).100 Use of these agents for foam sclerotherapy is not currently approved by the US Food and Drug Administration; however, such therapy is used routinely to treat CVI. About 20% to 50% of people whove had DVT develop post-thrombotic syndrome, usually within one to two years. Risk factors include: Sometimes, CVI cant be prevented. ankles swelling spots brown disease leg feet veins vein liver lower discoloration swollen near varicose causes venous extremity medical spider Prospective evaluation of the clinical deterioration in post-thrombotic limbs. Clinical signs of chronic venous insufficiency include: Clinical features of venous insufficiency If conservative measures fail or provide an unsatisfactory response, further treatment should be considered on the basis of anatomic and pathophysiologic features (Figure 7). Necas M. Duplex ultrasound in the assessment of lower extremity venous insufficiency. DGA declares that he has no competing interests. Microthrombectomy reduces postsclerotherapy pigmentation: multicenter randomized trial. are usually classified as the first level in the grading system, C1 disease. Your feedback has been submitted successfully. This condition is known as cellulitis, which is dangerous if not treated right away. Figure 1. This article reviews clinical aspects of CVI, with a focus on the diagnostic and therapeutic options, and places these in context of the Clinical Practice Guidelines (CPG) of the Society for Vascular Surgery and American Venous Forum of 2011, which used best evidence-based practice, and applied a grading system.18. The pressure is determined in the upright posture at rest and after exercise, such as during toe raises. Prospective randomized controlled trial: conventional versus powered phlebectomy. However, there is some concern that this pressure may not accurately reflect the pressure within the deep system.75 This technique is seldom used in clinical practice because of its invasive nature, potential limitations, and alternative diagnostic modalities. Are Inflammatory Biomarkers Increased in Varicose Vein Blood? Often, As venous insufficiency progresses, swelling is seen. The significance of calf muscle pump function in venous ulceration. The stages are based on clinical signs, which are things your provider can see or feel when they examine your legs. Once present, varicose veins will not usually go away. As the skin changes progress the lower leg becomes browner, the skin drier and more fragile. If theyre very painful, they may be infected. From symptoms to leg edema: efficacy of Daflon 500 mg. The valves prevent blood from being forced more distally within the deep system or through perforator veins into the superficial system. Pain is typical of deep venous insufficiency. Chronic deep venous obstruction: definition, prevalence, diagnosis, management. Photoplethysmography may be used to assess the time required to refill the veins within the dermis or the venous refill time. It usually spares involvement of the feet, often with a cuff of tissue at the ankle. It instead flows backward, a situation known as venous reflux. Spontaneous bleeding after a shower can occur because the warmth of the shower causes the vessels to dilate and the skin to soften. Randomised, double blind, multicentre, placebo controlled study of sulodexide in the treatment of venous leg ulcers. Now scheduling for ages 6 months and up, Coming to a Cleveland Clinic location? There may also be tenderness along varicose veins because of venous distention. And finally, P stands for pathophysiology. Additionally, spider veins are very common such that over half the US population has spider veins. Often, varicose veins are symptomatic causing heavy, tired, sore, itchy legs. As a result, these veins cant manage blood flow as well as they should, and its harder for blood in your legs to return to your heart. CEAP Classification of Chronic Venous Disease. You may not have all of these issues at once. Traditional surgical techniques and newer interventional methods are often reserved for unsatisfactory response to conservative measures, although earlier use of venous ablation should be considered in symptomatic patients. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. Additionally, leg swelling can be worse after travel. Direct noninvsive tests (duplex scan) for the evaluation of chronic venous obstruction and valvular incompetence. The infection could spread to nearby tissue. venous veins varicose figure Topical treatments are helpful; however, these patients do require treatment of their venous insufficiency to control their symptoms. Venography may be used to directly visualize the venous system by either an ascending or descending approach (Figure 5).69 Ascending venography involves injection of contrast in the dorsum of the foot with visualization of contrast-traveling cephalad in the deep venous system of the limb. Additionally, consult a physician if you have any medical conditions that makes your blood clot abnormally (cancer, recent pregnancy, immobility, recent surgery). 2003;158(5):44856. Varicose veins or a family history of varicose veins. If you have both CVI and PAD, your provider will advise you on treatment methods and precautions you need to take with compression therapy. The principle for using these venoactive drugs is to improve venous tone and capillary permeability, although a precise mechanism of action for these drugs has not been full elucidated. 
 Some procedures and surgeries can target and remove the damaged veins so that blood doesnt flow through them anymore. The objective is to provide graded external compression to the leg and oppose the hydrostatic forces of venous hypertension. RAK has received NIH research funds greater than 6 figures USD. Similarly, chronic venous insufficiency cant be cured. With a structured regimen of compression therapy, complete ulcer healing can be achieved in >90% of patient with ulcers at a mean of 5.3 months.78 Several studies have investigated the hemodynamic benefits of compression therapy in patients with CVI.
Some procedures and surgeries can target and remove the damaged veins so that blood doesnt flow through them anymore. The objective is to provide graded external compression to the leg and oppose the hydrostatic forces of venous hypertension. RAK has received NIH research funds greater than 6 figures USD. Similarly, chronic venous insufficiency cant be cured. With a structured regimen of compression therapy, complete ulcer healing can be achieved in >90% of patient with ulcers at a mean of 5.3 months.78 Several studies have investigated the hemodynamic benefits of compression therapy in patients with CVI.  Treatment cant reverse the damage to your vein valves. Youn YJ, Lee J. The rate of complication development is not known. These modalities have been largely replaced by venous duplex imaging but may be performed if venous reconstruction is being contemplated. CVD is a common problem with a significant impact on both afflicted individuals and the healthcare system. Ambulatory venous pressure has been shown to be valuable in assessing the severity and clinical outcomes in CVI.74 The mean ambulatory venous pressure and refill time are the most useful parameters. Obstruction of the deep veins may limit the outflow of blood, causing increased venous pressure with muscle contraction, and lead to secondary muscle pump dysfunction. This discomfort is thought to be produced by increased intracompartmental and subcutaneous volume and pressure. Finally, other regional considerations should be made, such as ruptured popliteal cyst, soft tissue hematoma or mass, exertional compartment syndrome, or gastrocnemius tear. E stands for etiology. corona phlebectatica (malleolar flare or ankle flare). CVI can happen due to damage in any of your leg veins. CVI often indicates the more advanced forms of venous disorders, including manifestations such as hyperpigmentation, venous eczema, lipodermatosclerosis, atrophie blanche, and healed or active ulcers. Generally, there is a strong genetic cause to varicose veins. Estimates suggest rates as high as 50% in some populations. Your provider can assess your risk factors and help you lower them. The term CVI is usually reserved for more advanced disease involving edema, skin changes, or frank ulcers. Treatment for chronic venous sufficiency involves lifestyle changes and compression therapy. Additionally, the ulcers often are very moist and will soak through dressings. The presence of venous obstruction because of chronic deep vein thrombosis or venous stenosis may be directly visualized or inferred from alteration in spontaneous flow characteristics. Critical disorders to consider are lymphedema, lipedema, and the combined disorder of lipolymphedema. Then, systemic causes of edema need to be considered, such as heart failure, nephrosis, liver disease, or endocrine disorders. What do the patients veins look like? Flaking or itching skin on your legs or feet. Evaluation of therapeutic compression stockings in the treatment of chronic venous insufficiency. Venous stasis ulcers dont heal easily, and they can become infected. Photoplethysmography in the assessment of venous insufficiency. Chronic venous insufficiency (CVI) is a form of venous disease that occurs when veins in your legs are damaged. Failure of microvenous valves in small superficial veins is a key to the skin changes of venous insufficiency. The presence of active or healed ulcers, typically in a distribution near the medial aspect of the ankle with GSV reflux or lateral aspects of the ankle with small saphenous vein reflux, may be seen with more advanced disease.48. A US study found ethnic whites had a higher rate of venous insufficiency compared to Hispanics, African Americans, and Asians. Arteriosclerosis, Thrombosis, and Vascular Biology (ATVB), Journal of the American Heart Association (JAHA), Stroke: Vascular and Interventional Neurology, Customer Service and Ordering Information, Basic, Translational, and Clinical Research. Risk factors found to be associated with CVI include age, sex, a family history of varicose veins, obesity, pregnancy, phlebitis, and previous leg injury.9,10 There are also environmental or behavioral factors associated with CVI, such as prolonged standing and perhaps a sitting posture at work.10,11, The more serious consequences of CVI, such as venous ulcers, have an estimated prevalence of 0.3%, although active or healed ulcers are seen in 1.0% of the adult population.12 It has been estimated that approximately 2.5 million people experience CVI in the United States, and of those 20% develop venous ulcers.13 The overall prognosis of venous ulcers is poor, because delayed healing and recurrent ulceration are very common.14 The socioeconomic impact of venous ulceration is dramatic because of an impaired ability to engage in social and occupational activities, reducing the quality of life and imposing financial constraints. Optimal therapy for advanced chronic venous insufficiency. The EF is a measure of the calf muscle pump function.
Treatment cant reverse the damage to your vein valves. Youn YJ, Lee J. The rate of complication development is not known. These modalities have been largely replaced by venous duplex imaging but may be performed if venous reconstruction is being contemplated. CVD is a common problem with a significant impact on both afflicted individuals and the healthcare system. Ambulatory venous pressure has been shown to be valuable in assessing the severity and clinical outcomes in CVI.74 The mean ambulatory venous pressure and refill time are the most useful parameters. Obstruction of the deep veins may limit the outflow of blood, causing increased venous pressure with muscle contraction, and lead to secondary muscle pump dysfunction. This discomfort is thought to be produced by increased intracompartmental and subcutaneous volume and pressure. Finally, other regional considerations should be made, such as ruptured popliteal cyst, soft tissue hematoma or mass, exertional compartment syndrome, or gastrocnemius tear. E stands for etiology. corona phlebectatica (malleolar flare or ankle flare). CVI can happen due to damage in any of your leg veins. CVI often indicates the more advanced forms of venous disorders, including manifestations such as hyperpigmentation, venous eczema, lipodermatosclerosis, atrophie blanche, and healed or active ulcers. Generally, there is a strong genetic cause to varicose veins. Estimates suggest rates as high as 50% in some populations. Your provider can assess your risk factors and help you lower them. The term CVI is usually reserved for more advanced disease involving edema, skin changes, or frank ulcers. Treatment for chronic venous sufficiency involves lifestyle changes and compression therapy. Additionally, the ulcers often are very moist and will soak through dressings. The presence of venous obstruction because of chronic deep vein thrombosis or venous stenosis may be directly visualized or inferred from alteration in spontaneous flow characteristics. Critical disorders to consider are lymphedema, lipedema, and the combined disorder of lipolymphedema. Then, systemic causes of edema need to be considered, such as heart failure, nephrosis, liver disease, or endocrine disorders. What do the patients veins look like? Flaking or itching skin on your legs or feet. Evaluation of therapeutic compression stockings in the treatment of chronic venous insufficiency. Venous stasis ulcers dont heal easily, and they can become infected. Photoplethysmography in the assessment of venous insufficiency. Chronic venous insufficiency (CVI) is a form of venous disease that occurs when veins in your legs are damaged. Failure of microvenous valves in small superficial veins is a key to the skin changes of venous insufficiency. The presence of active or healed ulcers, typically in a distribution near the medial aspect of the ankle with GSV reflux or lateral aspects of the ankle with small saphenous vein reflux, may be seen with more advanced disease.48. A US study found ethnic whites had a higher rate of venous insufficiency compared to Hispanics, African Americans, and Asians. Arteriosclerosis, Thrombosis, and Vascular Biology (ATVB), Journal of the American Heart Association (JAHA), Stroke: Vascular and Interventional Neurology, Customer Service and Ordering Information, Basic, Translational, and Clinical Research. Risk factors found to be associated with CVI include age, sex, a family history of varicose veins, obesity, pregnancy, phlebitis, and previous leg injury.9,10 There are also environmental or behavioral factors associated with CVI, such as prolonged standing and perhaps a sitting posture at work.10,11, The more serious consequences of CVI, such as venous ulcers, have an estimated prevalence of 0.3%, although active or healed ulcers are seen in 1.0% of the adult population.12 It has been estimated that approximately 2.5 million people experience CVI in the United States, and of those 20% develop venous ulcers.13 The overall prognosis of venous ulcers is poor, because delayed healing and recurrent ulceration are very common.14 The socioeconomic impact of venous ulceration is dramatic because of an impaired ability to engage in social and occupational activities, reducing the quality of life and imposing financial constraints. Optimal therapy for advanced chronic venous insufficiency. The EF is a measure of the calf muscle pump function.  It is important to realize that the same clinical manifestations may result from different pathogenic mechanisms, including incompetent valves, venous obstruction, muscle pump dysfunction, or a combination. News in Pathogenesis of Chronic Venous Insufficiency, Segregated Foxc2, NFATc1 and Connexin expression at normal developing venous valves, and Connexin-specific differences in the valve phenotypes of Cx37, Cx43, and Cx47 knockout mice, Chronic venous disease Part II: Proteolytic biomarkers in wound healing, Lymphatic transport in patients with chronic venous insufficiency and venous leg ulcers following sequential pneumatic compression, Management of Patients With Venous Leg Ulcers: Challenges and Current Best Practice, Pathophysiology of wound healing and alterations in venous leg ulcers-review, The Effectiveness of the Method Chiva in Patients with Chronic Venous Insufficiency and Comorbid Lesions: own Experience, Chronic venous disease and venous leg ulcers: An evidence-based update, Venous leg ulceration pathophysiology and evidence based treatment, Supervised exercise training as an adjunctive therapy for venous leg ulcers: study protocol for a randomised controlled trial, Venous leg ulcers: Impact and dysfunction of the venous system. August 2021. The Clinical, Etiology, Anatomic, Pathophysiology (CEAP) classification was developed by an international consensus conference to provide a basis of uniformity in reporting, diagnosing, and treating CVI (Table 1).40 The clinical classification has 7 categories (06) and is further categorized by the presence or absence of symptoms.
It is important to realize that the same clinical manifestations may result from different pathogenic mechanisms, including incompetent valves, venous obstruction, muscle pump dysfunction, or a combination. News in Pathogenesis of Chronic Venous Insufficiency, Segregated Foxc2, NFATc1 and Connexin expression at normal developing venous valves, and Connexin-specific differences in the valve phenotypes of Cx37, Cx43, and Cx47 knockout mice, Chronic venous disease Part II: Proteolytic biomarkers in wound healing, Lymphatic transport in patients with chronic venous insufficiency and venous leg ulcers following sequential pneumatic compression, Management of Patients With Venous Leg Ulcers: Challenges and Current Best Practice, Pathophysiology of wound healing and alterations in venous leg ulcers-review, The Effectiveness of the Method Chiva in Patients with Chronic Venous Insufficiency and Comorbid Lesions: own Experience, Chronic venous disease and venous leg ulcers: An evidence-based update, Venous leg ulceration pathophysiology and evidence based treatment, Supervised exercise training as an adjunctive therapy for venous leg ulcers: study protocol for a randomised controlled trial, Venous leg ulcers: Impact and dysfunction of the venous system. August 2021. The Clinical, Etiology, Anatomic, Pathophysiology (CEAP) classification was developed by an international consensus conference to provide a basis of uniformity in reporting, diagnosing, and treating CVI (Table 1).40 The clinical classification has 7 categories (06) and is further categorized by the presence or absence of symptoms.  Palpation along the course of dilated veins may reveal tenderness. Therefore, it is important to discuss any symptoms or concerns with a health care provider or vein specialist near you. Each year, about 1 in 50 adults with varicose veins go on to develop chronic venous insufficiency. Real epidemiology of varicose veins and chronic venous diseases: the San Valentino Vascular Screening Project. venous leg flare ankle dilated ulcer examination limb foot veins hypertension shaped due fan pattern around Figure 3. This process of isolated tributary reflux may contribute to progression of disease within the other superficial or deep venous segments.
Palpation along the course of dilated veins may reveal tenderness. Therefore, it is important to discuss any symptoms or concerns with a health care provider or vein specialist near you. Each year, about 1 in 50 adults with varicose veins go on to develop chronic venous insufficiency. Real epidemiology of varicose veins and chronic venous diseases: the San Valentino Vascular Screening Project. venous leg flare ankle dilated ulcer examination limb foot veins hypertension shaped due fan pattern around Figure 3. This process of isolated tributary reflux may contribute to progression of disease within the other superficial or deep venous segments.